5.6.2: Therapeutic Radiation
- Page ID
- 466606
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)- Distinguish between diagnostic and therapeutic radiation.
- Know the types of cancer treatments available.
- Recall the A/Z formats of a proton (particle) and gamma (ray).
- Compare/contrast external beam therapy and brachytherapy.
- Know the differences between proton and photon radiation.
- Realize the side effects of radiation therapy and medications available.
There are many techniques used to treat cancer. Surgery can be used to remove cancerous tumors inside or on the body. With chemotherapy, ingested or injected chemicals are used to kill rapidly dividing cells (cancerous and noncancerous). For more information regarding chemotherapy, please access this link. Other cancer treatment methods include immunotherapy, stem cell replacement, hormone therapy, and targeted therapy.
Patients diagnosed with cancer might be required to undergo chemotherapy or radiation therapy. Sometimes, both of these methods are used for a patient. In this picture, a female patient is receiving chemotherapy through an IV. She is participating in cooling therapy while receiving her treatment. By placing her hands and feet in cooling devices, this will lower her chances of losing her fingernails and toenails. Cold cap therapy is also now available for chemotherapy patients. Wearing this type of device increases a patient's chances of keeping his/her hair during chemotherapy.

Current therapeutic radiation applications involve the use of gamma, X-rays, or protons. Recently, some research facilities are investigating the use of alpha- or beta-tagged molecules to kill cancer cells. These molecules will target a cancer-related molecule on a tumor cell. Then, the alpha- or beta-tagged species will deliver its radiation to the tumor. Sr-89 (beta emitter) and Ra-223 (alpha emitter) have been used in clinical research trials of certain types of bone cancers.
Oncologists (specialists who treat patients with cancer) utilize radiation to help slow or cure the spread of cancer within individuals. Radiation is specifically applied to malignant tumors to shrink them in size. Medical professionals, mainly radiation oncologists, administer a variety of dosages to patients, contingent on factors such as the patient's current health, the concurrent use of other treatments, and the success of surgery.
External Beam Therapy (Photon and Proton Therapy)
External Beam Therapy (EBT) is a method of delivering a high-energy beam of radiation to the precise location of a patient's tumor. These beams can destroy cancer cells and with careful planning, preserve surrounding cells. Several beams of sub-lethal doses of radiation enter the body from different directions. The only place in the body where the beam is lethal is the spot where all the beams intersect. Before the EBT process, the patient is three-dimensionally mapped using CT scans and X-rays. The patient receives small tattoos to allow the therapist to line up the beams exactly. Alignment lasers are used to precisely locate the target. The video below illustrates the basic preparation and administration of external beam therapy.
Targeting Cancer - Radiation Therapy Treatment Process
Photon EBT utilizes either X-ray or gamma rays. An X-ray source would require a linear accelerator to produce high-energy electrons. In contrast, a gamma source incorporates a radioactive isotope (like Co-60). Keep in mind both of these technologies use ionizing radiation. As a result, cancer patients must be monitored throughout their life because they are at an increased risk for developing other cancers such as leukemia. EBT is used to treat many cancers such as:
- Breast cancer
- Colorectal cancer
- Head and neck cancer
- Lung cancer
- Prostate cancer
The majority of radiation patients receive photon EBT. The smaller size of this machine makes this therapy an option for all sizes of hospitals and cancer treatment centers. The equipment required for Photon EBT costs approximately three million dollars. The size and the price of this technology enables smaller facilities to keep their patients closer to home during treatment
In the past ten years, another method of radiation treatment involving protons has become more widely available. This type of therapy requires a cyclotron to generate proton beams (recall, a proton is an ionized H-1 isotope). As compared to X-rays or gamma rays (photon therapy), protons are very heavy. Today's proton facilities occupy large plots of land to house the medical cyclotron (the size of a football field that is three stories high). With a price tag of 150-200 million dollars, these facilities are sporadically located in the United States.

At this time, research facilities are working on miniaturizing proton generators. An ideal technology would reduce the cost from hundreds of millions of dollars to about twenty to thirty million per device. This would make proton therapy more available and convenient for patients.
Proton Therapy versus Photon Therapy
There are many advantages to choosing proton therapy over photon therapy. Unlike photon radiation, proton beams will only penetrate to the depth of the tumor and not pass through the entire body. This reduces the overall toxicity dose. In addition, fewer treatments are required for proton therapy patients than photon therapy.Unfortunately, proton therapy is more expensive than photon therapy and less common. Once approved by a facility and medical insurance, a patient may have to move temporarily to a larger city to receive treatment. Some forms of cancer have never been clinically treated with proton therapy (namely, breast cancer). Patients desiring proton therapy might not be able to receive type of therapy due to lack of research.
Brachytherapy
The Greek term brachy means to travel a short distance. This type of radiation involves placing ionizing pellets(seeds) or rods directly at the tumor. Photons (in the form of x-ray or gamma ray) are produced inside the body and will penetrate throughout this particular area localizing the radiation. Pellets are surgically implanted while rods can be temporarily inserted to produce radiation internally. With pellets/seeds, the patient will remain radioactive as long as these devices remain inside the body. People undergoing this type of radiotherapy need to be aware of their constant emission of radiation. Radiation that is administered through rods connected to a photon device will disperse energy immediately and not leave the patient radioactive.
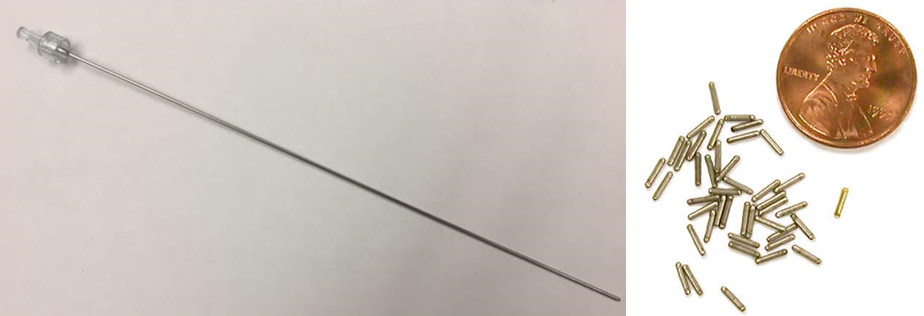
Brachytherapy is widely used in the treatment of cancers involving reproductive organs. Because the radiation is isolated internally, patients are less likely to experience side effects when receiving this type of treatment. Cancers that have been treated with brachytherapy are shown below:
- Prostate
- Breast
- Esophageal
- Lung
- Uterine
- Anal/Rectal
- Sarcomas
- Head and neck
| Radionuclide | Type | Half-life |
|---|---|---|
| Cesium-131 (131Cs) | Electron Capture, ε | 9.7 days |
| Cesium-137 (137Cs) | β−- particles, γ-rays | 30.17 years |
| Cobalt-60 (60Co) | β−- particles, γ-rays | 5.26 years |
| Iridium-192 (192Ir) | γ-rays | 73.8 days |
| Iodine-125 (125I) | Electron Capture, ε | 59.6 days |
| Palladium-103 (103Pd) | Electron Capture, ε | 17.0 days |
| Ruthenium-106 (106Ru) | β−- particles | 1.02 years |
| Radium-226 (226Ra) | β−- particles | 1599 years |
Side Effects of Radiation Therapy
Patients receiving radiation therapy can experience a variety of side effects. For example, sterility could occur if reproductive organs are irradiated. Skin that has been irradiated can appear dry and feel itchy. Some patients will loose sensation in the irradiated area. Radiation can affect the production of white and red blood cells. A reduction of white blood cells results in immunity disorders. Red blood cell lose causes anemia. Gastrointestinal issues such as diarrhea and nausea are common during radiation therapy. Some patients will lose hair as well. Lastly, dry mouth and tooth decay are prevalent during radiation treatments.
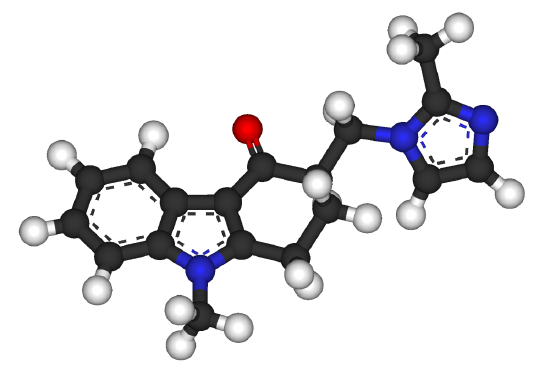
Medications are available to alleviate symptoms of radiation therapy. Narcotics can be prescribed to help alleviate intense pain. Prescription medications like zofran and phenergan can help with nausea. Special mouthwashes have been formulated to reduce dry mouth and cavities.
.jpg?revision=1&size=bestfit&width=243&height=324)
Radiation therapy can cause hair loss, but hair is only lost in the area being treated. For instance, radiation to your head may cause you to lose some or all the hair on your head (even eyebrows and lashes), but if you get treatment to your hip, you won’t lose the hair on your head.
Access to Radiotherapy
For those countries who do not have access to nuclear technologies, the International Atomic Energy Agency (IAEA) provides support and technical assistance to its member countries. When nations chose to join the IAEA, then they will gain nuclear materials and technologies for energy, medical, industrial, and agriculture purposes. Once accepted into the IAEA, a country must allow weapons inspectors to monitor any equipment that could be used to make nuclear weapons. The IAEA does not allow countries that do not have nuclear weapons to obtain them.
IAEA video: Fighting Cervical Cancer: A Fair Chance for Every Woman Around the World
References
- https://www.cancer.gov/about-cancer/treatment/types
- https://weillcornellgucancer.org/201...-cancer-cells/
- http://www.proton-therapy.org/zapper.htm
- www.brachytherapy.com/
- https://www.iaea.org/
Contributors and Attributions
Paul Flowers (University of North Carolina - Pembroke), Klaus Theopold (University of Delaware) and Richard Langley (Stephen F. Austin State University) with contributing authors. Textbook content produced by OpenStax College is licensed under a Creative Commons Attribution License 4.0 license. Download for free at http://cnx.org/contents/85abf193-2bd...a7ac8df6@9.110).
- Emma Gibney (Furman University)

