4.4: Treatments for Type II Diabetes
- Page ID
- 473705
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
Importantly, the treatments for Type I diabetes all involve injections as they are large peptides that would not be suitable as oral agents since they would not survive in the stomach or be absorbed by small intestine without cleavage/modification. Type II diabetes usually emerges as a loss of sensitivity to insulin, and introduction of more insulin may not be the most efficient method to reduce blood sugar concentrations. In these cases, there have been a number of small molecules or oral agents developed.
Multiple Blood Glucose Lowering Effects: Biguanides
Biguanides were originally identified in the 1840s from herbs such as the French lilac, which is rich in guanidine derivatives. However, from an array of these guanidine compounds, several had significant adverse effects, and were not advanced. However, they were revisited again in the 1950s for treatment of diabetes, and the compound metformin was explored further. Chemically, a biguanide involves the linkage of two guanidine molecules, and metformin is capped with two methyl- groups on one end. Other compounds such as butformin (capped with a butyl group) or phenformin (capped with a phenyl group) presented with several side effects and were found to be less useful in treating diabetes. (Figure 4.9) Metformin is a relatively planar molecule, and is monoprotonated at neutral pH. It has approximately 50% oral bioavailability and a tmax of ~2.5 h. The mechanism of action for metformin is still heavily debated and it has been described to have at least three key effects:
- Reduced hepatic glucose formation (blocking gluconeogenesis)
- Reduced intestinal absorption of glucose
- Increased insulin sensitivity

Physiological and biochemical studies have revealed that metformin enters the liver via action of OCT1 (organic cation transporter) and ultimately blocks the electron transport chain which is required for oxidative phosphorylation and energy generation. (Figure 4.10) Since the key molecule in electron shuttling and energy generation (NADPH) deposits electrons in the ETC to re-generate NADP+, shutting down the ETC leads to build up of NADPH in the cell. Excess NADPH causes multiple biochemical effects and signals the cells to stop converting glycogen to glucose. Additionally, the build up of NADPH can lead to NADPH reducing pyruvate to form lactic acid. As such, one of the potential adverse effects of metformin is lactic acidosis.

Metformin is ultimately excreted by the kidneys and because of these effects, it is usually discontinued if a patient is admitted to the hospital for a condition where a CT scan may be likely. This is because the contrast agent is also processed by the kidneys. If both metformin and contrast agent are administered, since they are competing for renal clearance, metformin may remain in the body longer, and lead to excess concentrations and lactic acidosis.
Increasing Insulin Release: Sulfonylureas
Sulfonylureas are drugs that contain a sulfonylurea functional group (usually neighbouring an aryl ring) and bind the aptly named, sulfonylurea receptors(SURs) in the pancreas. (Fig 4.11) SUR proteins are ABC transporters that are part of a larger complex of ATP-sensitive potassium channels (called KATP channels) and act as gatekeepers of releasing insulin. These drugs have been utilized for several decades and are relatively inexpensive. Under normal function, the presence of glucose in the pancreas cells also leads to high concentration of intracellular ATP. High levels of ATP block the KATP channel, which leads to membrane depolarization triggering voltage gated Ca2+ channels and Ca2+ ion influx. As shown previously (Figure 4.3), the introduction of Ca2+ leads to insulin release.

Administering sulfonylurea drugs produces the same response as high levels of intracellular ATP. Specifically, the sulfonylurea will bind the KATP channel, leading to membrane depolarization and Ca2+ influx. This essentially decouples the release of insulin from blood glucose concentrations. However, it should be noted that if excess sulfonylureas are administered, this can cause blood glucose concentrations to drop dramatically.
Some additional side effects of sulfonylureas are that they can cause the patient to gain weight (as sulfonylureas lead to additional insulin release, which triggers cells throughout the body to uptake more glucose). Furthermore, KATP channels are also located in other tissues in the body including the heart, and non-specific binding of sulfonylureas can lead to an increased risk of cardiac events.
Increasing Insulin Release: Meglitinides
Meglitinides have a similar mechanism of action as sulfonylureas – they bind to the KATP channel (at a different site on the SUR protein compared to sulfonylurea drugs). (Figure 4.12) However, the interaction between meglitinides and the SUR protein is not as strong as the sulfonylurea-SUR binding. This results in a relatively weaker effect that has a shorter duration of action. This reduced activity can be very useful, since it can lead to more flexibility in treatment options and meglitinides are not associated with adverse cardiovascular events. Meglitinides also present as a suitable option in case the patient is allergic to sulfonylureas.

Increasing Insulin Production: Dipeptidyl Peptidase 4 (DPP-4) Inhibitors
In addition to the hormones produced by the pancreas, there are also hormones produced by the small intestine called incretins (including GIP and GLP1). These incretins stimulate the body to prepare for food intake as well as insulin production/release. These incretins are very rapidly degraded by dipeptidyl peptidase 4 (DDP-4). Prolonging the effects of GIP/GLP1 (by inhibiting DDP-4 with small molecules) can increase insulin levels in the body as well as other digestion and absorption effects. DDP-4 inhibitors engage with DPP-4 at the GLP1 interaction site, and they are considered protein-protein interaction inhibitors. Several drugs contain azolopyrimidines which are important for hydrogen bonding interactions within the binding site. (Figure 4.13)

One side effect of these drugs is that they are usually associated with weight loss (although they lead to increased insulin release as with sulfonylureas ore meglitinides). This is because the prolonged incretin lifetime also increases feelings of satiety that usually suppresses diet and therefore reduce caloric intake.
Increasing Insulin Production: GLP1 Agonists
Similar to the mechanism with DDP-4 inhibitors, GLP1 agonists involve directly injecting the incretin GLP1 (comparable to injecting the hormone insulin in Type 1 Diabetes). GLP1 is preferred over GIP since it has more potent effects. There are two peptide backbones for these drugs, which are based on GLP1 and exendin-4 (originally isolated from the venom of the Gila monster reptile). (Figure 4.14) Since it is not a mammalian incretin, exendin-4 is not a substrate for DDP-4 and has longer life-time. As with DDP-4 inhibitors, these drugs slow the digestion of food, increase insulin output, and increase the feelings of satiety.

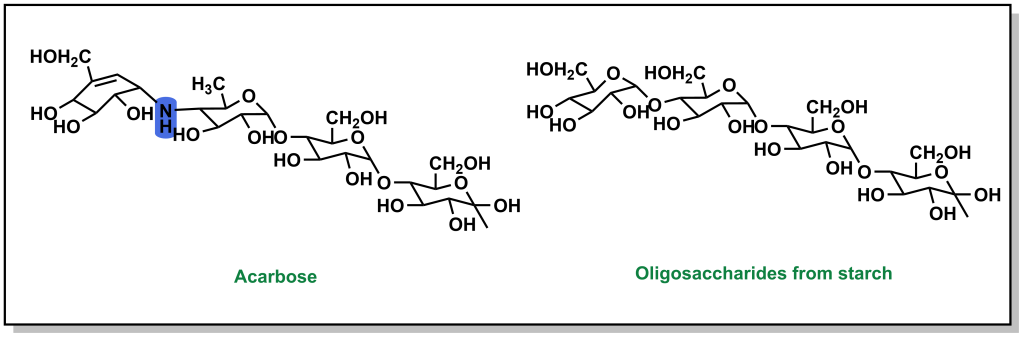
Blocking Glucose Absorption: α-Glucosidase Inhibitors
Absorption of carbohydrates occurs in the small intestine. However, blocking carbohydrate absorption can act as a preventative measure to reduce blood glucose concentrations. Large oligosaccharides cannot be directly absorbed and need to be cleaved into monosaccharides. This occurs by the action of α-glucosidases which are present at the small intestinal brush border. The drug, acarbose, is structurally very similar to oligosaccharides, but has a substantially higher affinity for α-glucosidase and is also non-cleavable. This leads to competitively blocking the active site of α-glucosidase, which prevents cleavage of oligosaccharides into monosaccharides, which subsequently blocks their absorption. These inhibitors can be more effective than traditional sulfonylureas, because they aim to prevent the spike in blood glucose levels proactively, as opposed to dealing with high concentrations after consumption.
Blocking Glucose Re-absorption: SGLT-2 Inhibitors
Since Type 2 diabetic patients have a higher concentration of glucose in the blood, this will result in higher concentrations of glucose in the kidneys. The nephrons of the kidneys are designed to reabsorb glucose via sodium glucose L-transporters (largely performed by SGLT-2 transporters). (Figure 4.16) This function is physiologically beneficial since it helps retain nutrients. However, blocking these transporters in Type II diabetic patients can reduce blood glucose levels.

Phlorizin is the first drug for this purpose and consists of a glucose moiety linked to a system of two phenyl rings (the “aglycone” moiety) that is connected by an ethylene bridge. (Figure 4.17)

Indirect Blood Glucose Reduction: Blocking Triglycerides with Thiazolidinediones / Glitazones
Thiazolidinediones, also called glitazones, encourage cells to switch to carbohydrates / glucose as the principal energy source, which ultimately lowers blood glucose levels. (Figure 4.18)

These drugs are agonists for PPARγ (peroxisome proliferator-activated receptor gamma), which is a transcription factor that complexes with retinoid X receptor (RXR). The end result is increased gene expression that will store fatty acids (reducing free fatty acids in blood circulation) and causing an increased cellular dependence on glucose. GLUT4 is an additional gene target for PPARγ, leading to increased glucose into cells. (Figure 4.19) However, it should be noted that the increased fatty acid storage is also correlated with reduced osteoblast formation, and there is a decrease in bone mineral density and increase risk of fractures with prolonged use of thiazolidinediones.



