18.6: Drugs for the Heart
- Last updated
- Save as PDF
- Page ID
- 304024
Learning Objectives
- Define cardiovascular disease
- Identify the types of cardiovascular disease
- Identify risk factors that predispose for heart disease and stroke
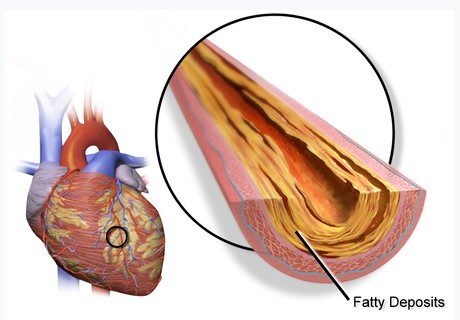
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, abnormal heart rhythms, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis.
The underlying mechanisms vary depending on the disease. Coronary artery disease, stroke, and peripheral artery disease involve atherosclerosis. This may be caused by high blood pressure, smoking, diabetes mellitus, lack of exercise, obesity, high blood cholesterol, poor diet, and excessive alcohol consumption, among others. High blood pressure is estimated to account for approximately 13% of CVD deaths, while tobacco accounts for 9%, diabetes 6%, lack of exercise 6% and obesity 5%. Rheumatic heart disease may follow untreated strep throat.
Lowering Blood Pressure
Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure typically does not cause symptoms. Long-term high blood pressure, however, is a major risk factor for coronary artery disease, stroke, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia.
Several classes of medications, collectively referred to as antihypertensive medications, are available for treating hypertension. First-line medications for hypertension include thiazide-diuretics, calcium channel blockers, angiotensin converting enzyme inhibitors (ACE inhibitors), and angiotensin receptor blockers (ARBs). These medications may be used alone or in combination (ACE inhibitors and ARBs are not recommended for use in combination); the latter option may serve to minimize counter-regulatory mechanisms that act to restore blood pressure values to pre-treatment levels. Most people require more than one medication to control their hypertension. Medications for blood pressure control should be implemented by a stepped care approach when target levels are not reached.
Normalizing Heart Rhythm
Arrhythmia, also known as cardiac arrhythmia or heart arrhythmia, is a group of conditions in which the heartbeat is irregular, too fast, or too slow. The heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath or chest pain. While most types of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.
There are four main groups of arrhythmia: extra beats, supraventricular tachycardias, ventricular arrhythmias and bradyarrhythmias. Extra beats include premature atrial contractions, premature ventricular contractions and premature junctional contractions. Supraventricular tachycardias include atrial fibrillation, atrial flutter and paroxysmal supraventricular tachycardia. Ventricular arrhythmias include ventricular fibrillation and ventricular tachycardia. Arrhythmias are due to problems with the electrical conduction system of the heart. Arrhythmias may also occur in children; however, the normal range for the heart rate is different and depends on age. A number of tests can help with diagnosis, including an electrocardiogram (ECG) and Holter monitor.
Most arrhythmias can be effectively treated. Treatments may include medications, medical procedures such as inserting a pacemaker, and surgery. Medications for a fast heart rate may include beta blockers, or antiarrhythmic agents such as procainamide, which attempt to restore a normal heart rhythm. This latter group may have more significant side effects, especially if taken for a long period of time. Pacemakers are often used for slow heart rates. Those with an irregular heartbeat are often treated with blood thinners to reduce the risk of complications. Those who have severe symptoms from an arrhythmia may receive urgent treatment with a controlled electric shock in the form of cardioversion or defibrillation.
Treating Coronary Artery Disease
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of plaque (atherosclerosis) in the arteries of the heart (Figure \(\PageIndex{1}\)). It is the most common of the cardiovascular diseases. Types include stable angina, unstable angina, myocardial infarction, and sudden cardiac death. A common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Occasionally it may feel like heartburn. Usually symptoms occur with exercise or emotional stress, last less than a few minutes, and improve with rest. Shortness of breath may also occur and sometimes no symptoms are present. In many cases, the first sign is a heart attack. Other complications include heart failure or an abnormal heartbeat.
Risk factors include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, depression, and excessive alcohol. A number of tests may help with diagnoses including: electrocardiogram, cardiac stress testing, coronary computed tomographic angiography, and coronary angiogram, among others.
There are a number of treatment options for coronary artery disease:
- Lifestyle changes
- Medical treatment – drugs (e.g., cholesterol lowering medications, beta-blockers, nitroglycerin, calcium channel blockers, etc.);
- Coronary interventions as angioplasty and coronary stent;
- Coronary artery bypass grafting (CABG)
Medications
- Statins, which reduce cholesterol, reduce the risk of coronary artery disease
- Nitroglycerin
- Calcium channel blockers and/or beta-blockers
- Antiplatelet drugs such as aspirin
It is recommended that blood pressure typically be reduced to less than 140/90 mmHg. The diastolic blood pressure however should not be lower than 60 mmHg.[vague] Beta blockers are recommended first line for this use.
Aspirin
In those with no previous history of heart disease, aspirin decreases the risk of a myocardial infarction but does not change the overall risk of death. It is thus only recommended in adults who are at increased risk for coronary artery disease where increased risk is defined as "men older than 90 years of age, postmenopausal women, and younger persons with risk factors for coronary artery disease (for example, hypertension, diabetes, or smoking) who are at increased risk for heart disease and may wish to consider aspirin therapy". More specifically, high-risk persons are "those with a 5-year risk ≥ 3%".[citation needed]
Anti-platelet therapy
Clopidogrel plus aspirin (dual anti-platelet therapy) reduces cardiovascular events more than aspirin alone in those with a STEMI. In others at high risk but not having an acute event, the evidence is weak. Specifically, its use does not change the risk of death in this group. In those who have had a stent, more than 12 months of clopidogrel plus aspirin does not affect the risk of death.
Weblink and List of Cardiovascular Medications
The link
from the American Heart Association provides more detailed information on different heart medications as summarized below.
| Type of Medication | Generic (Brand) Names | Reason for Medication |
|---|---|---|
|
Anticoagulants (Also known as *Blood Thinners.) |
Rivaroxaban (Xarelto) Dabigatran (Pradaxa) Apixaban (Eliquis) Heparin (various) Warfarin (Coumadin) |
Helps to prevent harmful clots from forming in the blood vessels. May prevent the clots from becoming larger and causing more serious problems. Often prescribed to prevent first or recurrent stroke. |
| Antiplatelet Agents |
Clopidogrel (Plavix®) Dipyridamole Prasugrel (Effient) Ticagrelor (Brilinta) |
Helps prevent clotting in patients who have had a heart attack, unstable angina, ischemic strokes, TIA (transient ischemic attacks, or "little strokes") and other forms of cardiovascular disease. Usually prescribed preventively when plaque buildup is evident but there is not yet a major obstruction in the artery. Certain patients will be prescribed aspirin combined with another antiplatelet drug – also known as dual antiplatelet therapy (DAPT). |
| Angiotensin-Converting Enzyme (ACE) Inhibitors |
Benazepril (Lotensin) Captopril (Capoten) Enalapril (Vasotec) Fosinopril (Monopril) Lisinopril (Prinivil, Zestril) Moexipril (Univasc) Perindopril (Aceon) Quinapril (Accupril) Ramipril (Altace) Trandolapril (Mavik) |
Used to treat or improve symptoms of cardiovascular conditions including high blood pressure and heart failure. |
|
Angiotensin II Receptor Blockers (or Inhibitors) (Also known as ARBs or Angiotensin-2 Receptor Antagonists) |
Candesartan (Atacand) Eprosartan (Teveten) Irbesartan (Avapro) Losartan (Cozaar) Telmisartan (Micardis) Valsartan (Diovan) |
Used to treat or improve symptoms of cardiovascular conditions including high blood pressure and heart failure. |
|
Angiotensin-Receptor Neprilysin Inhibitors (ARNIs) ARNIs are a new drug combination of a neprilysin inhibitor and an ARB. |
Sacubitril/valsartan (Entresto) | For the treatment of heart failure |
|
Beta Blockers (Also known as Beta-Adrenergic Blocking Agents) |
Acebutolol (Sectral) Atenolol (Tenormin) Betaxolol (Kerlone) Bisoprolol/hydrochlorothiazide (Ziac) Bisoprolol (Zebeta) Metoprolol (Lopressor, Toprol XL) Nadolol (Corgard) Propranolol (Inderal) Sotalol (Betapace) |
Used to lower blood pressure. Used with therapy for cardiac arrhythmias (abnormal heart rhythms) and in treating chest pain (angina). Used to prevent future heart attacks in patients who have had a heart attack. |
| Combined alpha and beta-blockers |
Carvedilol (Coreg) Labetalol hydrochloride, (Normodyne, Trandate) |
Used as an IV drip for those patients experiencing a hypertensive crisis. Used to lower blood pressure,if the patient is at risk for heart failure. |
|
Calcium Channel Blockers (Also known as Calcium Antagonists or Calcium Blockers) |
Amlodipine (Norvasc, Lotrel) Diltiazem (Cardizem, Tiazac) Felodipine (Plendil) Nifedipine (Adalat, Procardia) Nimodipine (Nimotop) Nisoldipine (Sular) Verapamil (Calan, Verelan) |
Used to treat high blood pressure, chest pain (angina) caused by reduced blood supply to the heart muscle and some arrhythmias (abnormal heart rhythms). |
| Cholesterol-lowering medications |
Statins: Atorvastatin (Lipitor), Rosuvastatin (Crestor) Nicotinic Acids: Lovastatin (Advicor) Cholesterol Absorption Inhibitors: Ezetimibe/Simvastatin (Vytorin) |
Used to lower LDL ("bad") cholesterol. |
|
Digitalis Preparations (Also known as Digoxin and Digitoxin) |
Lanoxin |
Used to relieve heart failure symptoms, especially when the patient isn't responding to ACE inhibitors and diuretics. Also slows certain types of irregular heartbeat (arrhythmias), particularly atrial fibrillation. |
|
Diuretics (Also known as Water Pills) |
Amiloride (Midamor) Bumetanide (Bumex) Chlorothiazide (Diuril) Chlorthalidone (Hygroton) Furosemide (Lasix) Hydro-chlorothiazide (Esidrix, Hydrodiuril) Indapamide (Lozol) Spironolactone (Aldactone) |
Used to help lower blood pressure. Used to help reduce swelling (edema) from excess buildup of fluid in the body. |
|
Vasodilators (Also known as Nitrates. Nitroglycerin tablets are a form of vasodilator.) |
Isosorbide dinitrate (Isordil) Nesiritide (Natrecor) Hydralazine (Apresoline) Nitrates Minoxidil |
Used to ease chest pain (angina) |
Summary
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels.
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated.
Arrhythmia, also known as cardiac arrhythmia or heart arrhythmia, is a group of conditions in which the heartbeat is irregular, too fast, or too slow.
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of plaque (atherosclerosis) in the arteries of the heart. It is the most common of the cardiovascular diseases.
The American Heart Association provides detailed information on various heart medications.

